Flourish Founder Megan Nivens-Tannett had her first brush with mortality at a very young age when she learned that her grandmother was dying of breast cancer at 54. It was devastating to watch, but she was so young and never really understood the reason for her early death until later in life. Growing up, the word ‘cancer’ seemed to pepper conversations focused on her family’s health and never seemed to escape the family dialogue. Fueled by her mother’s sage advice on proactive healthcare, Megan committed to preventative measures. At 35, she breathed a sigh of relief when genetic tests revealed she was BRCA-negative, dodging what many consider the “ticking time bomb” in women’s health.

4 Generations of Megan’s family.
Flash forward to 2023: While Megan was waiting to be seen for her annual OBGYN appointment, a never-seen-before Nurse treated her and expressed a heightened interest when it came time to review her family history. The Nurse was intrigued, raised her eyebrows, and asked many questions, which took Megan by surprise. She saw her doctor yearly – and there’s never been such a heightened interest in her family history – until now. The Nurse eventually suggested that she take another genetic test, as advancements had come a long way since 2015. The results returned with unwanted information: Megan tested positive for a newly discovered breast cancer marker, the BARD1 mutation. Associated with the BRCA1 gene, the BARD1 gene typically helps prevent cancers, but the mutation increases the lifetime risk of breast cancer by as much as 40 percent. It’s a sobering turn of events, but Megan knows her story isn’t written yet. She has the information, and now she has the power to make informed choices for her future. And in doing so, she aims to rewrite her family’s troubled history with cancer once and for all.
Whether you’re browsing the internet, scrolling through social media, or just watching TV, you’ve probably noticed by now that influencers are everywhere. Youth and beauty have always been valued in American society, especially for women.
The constant focus on remaining young, toned, and beautiful translates to booming profits for the aesthetics industry, which is now creeping into traditional healthcare practices everywhere in the form of aesthetic treatments such as Botox, dermabrasion, CoolSculpting, chemical peels, jawline contouring, and other nonsurgical cosmetic procedures provided by primary healthcare providers.
“Is it just me, or do you see more jargon in the office about the side effects of fillers than you do about the health benefits of exercise? I feel like we’ve lost sight of what’s important.”
— Megan Nivens-Tannett
According to a report from the International Association for Physicians in Aesthetic Medicine, growth factors driving demand include celebrities and influencers, along with advances in non-invasive technologies that bypass the drawbacks of traditional surgeries. Another very significant driver is the Zoom Effect – the increase of video conferencing calls during the pandemic came paired with the unwanted side effect of everyone having a close-up view of not just each others’ faces, but their own, on a daily basis.
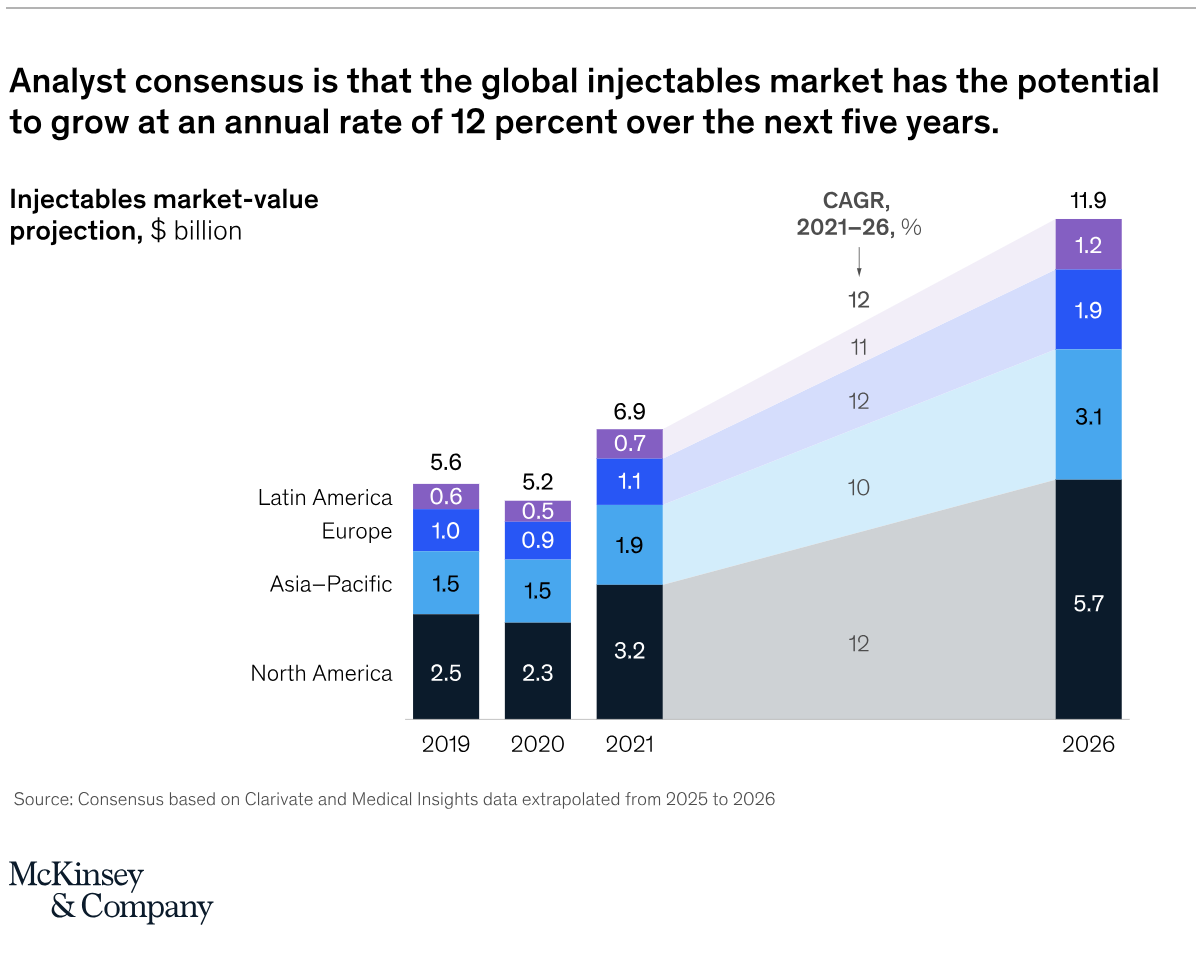
Because demand drives the adoption of new services, the aesthetic industry is in a major growth cycle. A 2021 McKinsey report entitled “From Extreme to Mainstream” predicts that the global aesthetic injectable market alone will grow by as much as 12% a year through 2026, with most of the growth taking place within the USA. From fillers and Botox to body contouring, cosmetic procedures are not just gaining popularity with image-conscious patients, but also with medical practices who recognize the potential for increased earnings by adding these services.
The Drawback of Healthcare Diversification
While medical aesthetics can be appealing to small medical practices, the addition of these services can lead to a greater push for profitable procedures not covered by health insurance over paying attention to patients’ legitimate healthcare concerns.
Adrienne Garbarino (MSN, FNP-BC, CRNP), owner of Huntsville-based Cove Telehealth for Women, noted that she has another concern with the recent increase of aesthetic procedures being offered by traditional medical practices: she feels like it confuses the message. “It already takes significant time and effort to be proactive and make an appointment, and you walk into a place where you want to focus on taking care of your health, but you’re bombarded with messages of ‘I’m not pretty enough because I need to look like that model on the Cool Sculpting advertisement.’” While she sees a place for these treatments and doesn’t object to them being offered, she feels that patients would be better served by keeping the cosmetic and medical parts of the office within separate spaces to create a distinct physical and psychological boundary between the two.
An article from the American Association of Aesthetic Medicine & Surgery illustrates another side effect of the growing focus on nonsurgical aesthetic treatments: nurses are leaving hospitals and clinics for the greener pastures of aesthetic nursing. The AAAMS’s promise of more lucrative careers for those who choose to switch from patient care to medical aesthetics foreshadows a shrinkage of the nursing field dedicated to healthcare in general. This is a problem: not only will the field of doctors and nurses be stretched more thin regarding time available for patient care, but for those remaining in traditional clinics, the increasing prioritization of the bottom line raises the likelihood that genuine health concerns will be increasingly overlooked as shrinking medical practices seek out more lucrative income sources.
With this knowledge, it’s important to be aware that for female patients especially, it is essential to take a proactive approach to one’s healthcare and pay attention to red flags.
Dawn’s story
With a strong family history of high cholesterol, high blood pressure, and hypothyroidism, Dawn followed in her parents’ footsteps and was already taking medications to treat each of the conditions. Her blood pressure and cholesterol were under control, but she had the feeling her thyroid medication wasn’t doing the job as effectively as it should have been. Despite her thyroid stimulating hormone (TSH) reading appearing to be on the high side of the “normal” range at 4.56 at the time of her last bloodwork, she was still losing a lot of hair and couldn’t lose weight despite daily exercise and a healthy diet. At her physical, the new nurse practitioner she saw barely touched her and merely glanced at the labs, saying everything was good, telling her to cut carbs, and sending her on her way in less than 15 minutes, including the overdue pap smear she requested.
Later, Dawn pulled out the prior year’s bloodwork and noticed that her TSH was previously 2.66, something completely overlooked by the nurse at her physical. Meanwhile, Dawn’s 26-year-old daughter, who also has hypothyroidism, saw a new doctor who took time to discuss her concerns and, after examining her TSH numbers, decided to double her thyroid medication dosage on the grounds that recent research recommends a level close to 2.0. That was the final straw for Dawn, who, tired of being ignored, called her daughter’s doctor to transfer her care over. It was time to make a change.
Medical gaslighting is real. You don’t have to accept it.
Like Dawn, Megan was tired of being ignored and decided to take control over her healthcare–after her own doctor brushed off her concerning family history, she took matters into her own hands and ordered a genetic cancer marker test on her own, which confirmed her fears when it came back positive for a BARD1 gene mutation.
Women’s health concerns are consistently dismissed by medical practitioners, who often tell female patients that it’s nothing to worry about, “in their head,” or that they just need to lose weight. According to the 2022 SHE Media Medical Gaslighting Survey, a whopping 72% of patients have experienced it, with 81% reporting that they felt misunderstood by medical professionals and 22% giving up on seeking treatment for their condition as a result. In addition, 73% of respondents reported that they’ve left an interaction with a medical practitioner doubting their experience or memory.
According to an article by Women’s Mental & Neurological Health (wmnHealth.org), research suggests that it takes women longer than men to receive a diagnosis, and if the problem isn’t something life-threatening that needs to be addressed immediately, women are told it’s just something they’re supposed to live with. That’s simply not acceptable.
Medical professionals may not even be aware of their medical gaslighting because it’s so ingrained in the profession. Whether or not it is intentional, it’s harmful: when it comes to preventing or addressing illness, ignorance is not bliss, especially when it involves delayed care that results in further complications down the road. Here are some tips to help you regain your power:
- Remove yourself from the situation: Gaslighting is stressful and can trigger powerful emotional reactions. It’s important to take a step back to process the experience before you choose to take action or make a medical decision that may not be in your best interests.
- Collect evidence: You deserve to be treated with respect and dignity. Take notes of your conversations with your doctor with time and date stamps. Creating documentation of discussions, timelines, and medical records will help you to advocate for yourself.
- Voice your concerns: This is where assertive language can help, as well as clear communication of your thoughts, beliefs, and needs. It’s important to talk to your healthcare providers calmly, respectfully, and proactively when addressing their dismissal of your medical concerns. It’s harder to dismiss someone’s concerns when they see that the patient has done their homework. Google isn’t all-knowing, but it can be a valuable tool to help gather research relating to your symptoms to share with your healthcare provider.
- Seek support: It’s easy to lose faith in the medical system when the people you’re supposed to rely on fail in their duties. There’s power in your support system: if you bring a friend or family member to a medical appointment, they can serve as an extra set of eyes and ears, not just for taking notes and providing moral support, but also observing the dynamic between the patient and medical provider to determine whether gaslighting is taking place.
- Change your healthcare provider: It’s hard to leave the familiar behind, but sometimes the familiar doesn’t work in your best interest. If you’re uncomfortable with your medical care (or lack thereof), you’ll be better off in the long run to make a switch to a medical professional who will advocate for you in the way that you need and deserve.
It can be challenging to find practitioners who are taking new patients, but it’s worth the effort to seek out a new practice that’s covered by your insurance and has positive reviews from patients. Facebook and Google reviews can be very informative–it’s important to read both the best and worst reviews to see whether there are any patterns. As the person who needs to care the most about your health, you deserve it. It’s your health and your life – time to take control.
Healthcare providers are frustrated too: Adrienne’s story
According to Adrienne Garbarino of Cove Telehealth for Women, most of the new patients who come to her practice tell her during their initial session that they’re there because of certain symptoms or ongoing chronic issues they know they have and their doctors or medical providers left them feeling unheard, not validated, and without solutions offered or directions given. She also noted that in many cases, these are hormonal issues that happen at the same time each month, and the solutions offered address symptoms, but not root causes. Her practice, on the other hand, focuses on what’s causing the symptoms and targets specific solutions including not just hormone therapy, but specific lifestyle changes.
As a former labor and delivery nurse and a family nurse practitioner, Adrienne knew she loved caring for women. Still, the increasing focus on the quantity of patients versus quality of care made her realize that she had to make a change: she said that she was never okay with seeing a patient for 15 minutes and showing them the door and faced complaints from management because she was always the slow provider. She later took a public health consultant position doing contract research work for the CDC, but Adrienne missed patient interactions and dreamed of opening her own practice that offered a more holistic approach to women’s healthcare.
While still working as a CDC contractor in February 2020, Adrienne gave birth to her son and experienced firsthand the hormonal disruptions that came with it such as anxiety, irritability, and mood swings. Her OBGYN offered the traditional treatment of birth control and antidepressants, which targets the symptoms but not the hormonal imbalances.
With some pre-existing knowledge in functional medicine, Adrienne was aware that this was not the cure she sought. She began studying functional medicine in depth as a means of self help, which led her to realize that she could use her knowledge to help other women. After working with other functional specialists in the area, she opened her own practice focusing on giving women the time and safe space to discuss their health concerns so they can get the treatment they need.
It’s unique in that it focuses specifically on the hormonal issues that impact women’s health on a day-to-day basis, including thyroid function, weight management, preventive care, and hormonal imbalances.
Cove Telehealth is also unique in that it does not accept insurance, although it does accept HSA and FSA payments. When asked why, Adrienne stated that it goes back to the way that insurance requires a traditional office structure with a high volume of patients. Because insurance revenue is very inconsistent and unpredictable and standard medical practices also have to support a large number of staff members, they have to focus on maximizing revenue by seeing as many patients as possible each day.
Cove Telehealth, on the other hand, offers a $180 new patient package to women between 19 and 64, including two one-hour sessions. During the first televisit, patients can take their time to fully discuss concerns and history, then following labs (billed to insurance), they return for a follow-up televisit in which the labs are reviewed, treatments are discussed, and a comprehensive plan is formulated to help the patient reach their goals. Patients can also schedule as-needed follow-up visits for $115 or a monthly subscription for patients with ongoing concerns for $95 a month.
It’s your life. Take control.
Your health and well-being can’t be taken for granted, and if you’re not comfortable with the care you’re getting, you shouldn’t have to accept it. You know your body and your symptoms–it’s not in your head and you deserve to be heard and respected.