Flourish Founder Megan Nivens-Tannett had her first brush with mortality at a very young age when she learned that her grandmother was dying of breast cancer at 54. It was devastating to watch, but she was so young and never really understood the reason for her early death until later in life. Growing up, the word ‘cancer’ seemed to pepper conversations focused on her family’s health and never seemed to escape the family dialogue. Fueled by her mother’s sage advice on proactive healthcare, Megan committed to preventative measures. At 35, she breathed a sigh of relief when genetic tests revealed she was BRCA-negative, dodging what many consider the “ticking time bomb” in women’s health.

4 Generations of Megan’s family.
Flash forward to 2023: While Megan was waiting to be seen for her annual OBGYN appointment, a never-seen-before Nurse treated her and expressed a heightened interest when it came time to review her family history. The Nurse was intrigued, raised her eyebrows, and asked many questions, which took Megan by surprise. She saw her doctor yearly – and there’s never been such a heightened interest in her family history – until now. The Nurse eventually suggested that she take another genetic test, as advancements had come a long way since 2015. The results returned with unwanted information: Megan tested positive for a newly discovered breast cancer marker, the BARD1 mutation. Associated with the BRCA1 gene, the BARD1 gene typically helps prevent cancers, but the mutation increases the lifetime risk of breast cancer by as much as 40 percent. It’s a sobering turn of events, but Megan knows her story isn’t written yet. She has the information, and now she has the power to make informed choices for her future. And in doing so, she aims to rewrite her family’s troubled history with cancer once and for all.
As part of our Women’s Health Initiative, Flourish is dedicated to promoting better physical and mental wellness for women, and what better time to do it than Breast Cancer and Women’s Health Month? Additionally, the recent COVID crisis highlighted the American healthcare system in new ways, highlighting strengths, weaknesses, and opportunities from both the provider and the patient perspectives as well as the changes that have taken place in access to and affordability of healthcare over recent years.
Stay with us as we launch our four-part series to raise awareness of women’s health issues, to encourage a proactive approach to your health and medical care, and to follow Megan’s journey. We’ll engage with local experts to learn how YOU can take control of your health, what resources may be available to you, how you can learn about your risks and more.
Cancer can’t be ignored: here’s why
CDC data says that cancer is the second leading cause of death in the United States, exceeded only by heart disease, with one of every five deaths in the U.S. due to cancer. Breast cancer accounts for about 30% of all new cancer cases in women each year in the U.S., with about 1 in 8 of U.S. women developing invasive breast cancer in the course of their life. It’s not just women though – a man’s lifetime risk of breast cancer is about 1 in 833. In fact, the National Cancer Institute notes that the most common type of cancer overall is breast cancer, followed by prostate cancer and lung cancer.
“An Uncle on my Dad’s side of the family developed breast cancer at the age of 35; if you think you’re immune, think again.”
— Megan Nivens-Tannett
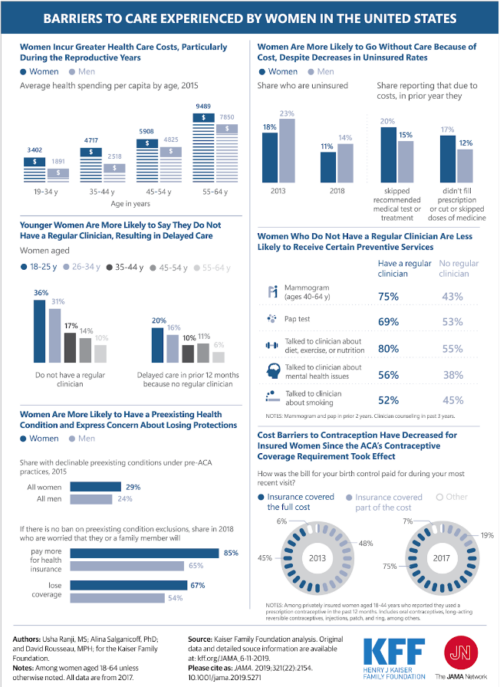
Major Issue: Affordability of Healthcare
One of the biggest issues that directly impacts healthcare in general, but especially women, is affordability. According to a recent study from the Commonwealth Fund, while the number and percentage of Americans lacking health insurance is falling to historic lows, inadequate insurance remains a big problem, with over two in five working-age adults struggling to afford care: 9% of respondents reported that they were uninsured, 11% had a gap in coverage over the past year, and 23% were underinsured, meaning that while they were insured, they wouldn’t have affordable access if an issue arose. In addition, 46% of respondents skipped or delayed care because of the cost and 42% reported having problems paying medical debt or were currently paying off medical debt.
The Affordable Care Act expanded coverage for women, barring plans from charging women higher premiums than men for the same level of coverage and no longer allowing them to disqualify women from coverage due to certain pre-existing conditions, including pregnancy and breast cancer.
Even for those with insurance, copays and high deductibles can deter seeking healthcare, leading people to delay treatment until the symptoms can no longer be ignored. This is especially true for those with low income and people of color, who continue to face additional financial barriers to quality healthcare.
It’s important to weigh your options: keep in mind that delaying disease prevention, detection, and treatment in the short term can translate into much higher costs down the road. Many resources are available to provide low or no-cost coverage at the county, state, and national levels if you know where to look. Here’s a helpful link that includes resources available to the public.
Complicating Factor: Recent Stresses on Medical Professionals
As we all know, the pandemic took a heavy toll on public health. At the same time, it deeply impacted the medical profession, driving huge numbers of professionals and support staff out of the industry. According to a March 2023 article from the Harvard Gazette, burnout and intent to leave remain major issues with not just individuals in clinical roles but also non-clinical support roles such as technicians, food service workers, and nursing assistants.
A recent report from the Peterson Center on Healthcare and KFF notes that while employment is recovering in the healthcare industry, many unfilled positions remain in the health sector. Unfortunately, this can also translate to longer waiting times, higher costs, and less comprehensive healthcare visits. A high turnover rate in private healthcare clinic staff can also lead to a loss of consistency with treatment – for instance, having a new nurse practitioner do your annual physical each year means that they’ll never have the opportunity to really get to know you as a patient (or as a person).
Women’s Health Matters
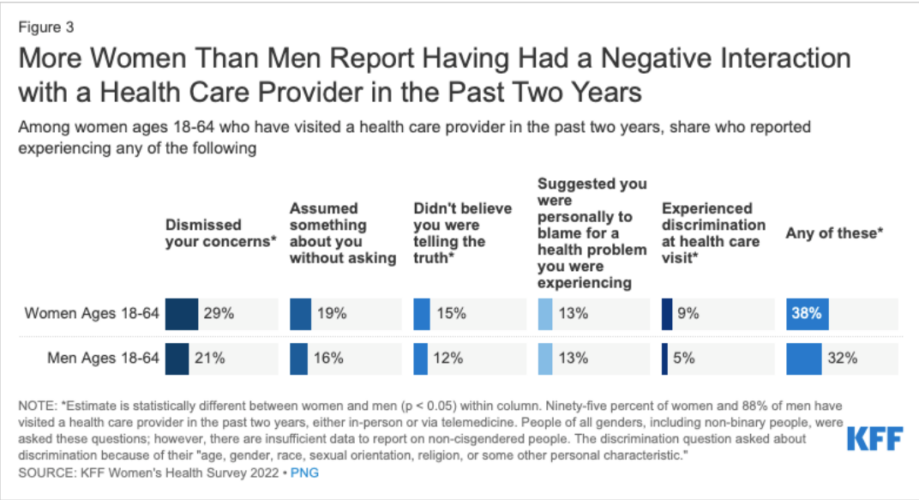
As the pandemic waned, women’s health came into sharper focus as recent legislation drew attention to the general lack of knowledge surrounding female biology. While written prior to the enactment of the Dobbs v. Jackson decision, this article from HIT Consultant does a good job of briefly summarizing some major healthcare issues faced by women today. We’ll explore a few of these topics in later installments, including telemedicine, taking control of one’s own health decisions, and destigmatizing female biology.
According to a 2022 report from McKinsey & Company, although women account for 80% of consumer purchasing decisions in the healthcare industry, women’s health has traditionally been considered a niche market and a mere subset of healthcare. Fortunately, that’s beginning to shift as healthcare providers increasingly recognize the opportunities presented by focusing more on women’s unique health needs. Still, women continue to face significant issues with respect to getting the care that they need from healthcare providers, especially when their symptoms aren’t visible.
Representation also matters
Women’s health has historically been overlooked in the medical research sphere, with research only recently beginning to focus more on women and people of color. In fact, women of childbearing age were excluded from Phase 1 and early Phase II drug trials in the late 1970s, leading to a shortage of data on how drugs affect women. In fact, the NIH didn’t even begin encouraging researchers to include women in studies until 1986, and not until 1993 were they required by law to include women and minorities.
Women in general have been historically underrepresented in medical research, but this applies to an even greater extent with people of color in medical research and clinical trials: the Association of American Medical Colleges states that Black patients account for only 5% of clinical trial participants in the United States, with the vast majority of products such as vaccines, therapeutic drugs, and devices tested primarily on White people – especially young and middle-aged men of European descent. This is a major problem, as these tests don’t take into consideration the enhanced risk factors common to certain ethnic groups, nor do they evaluate metabolic differences in the way drugs are processed depending on gender and ethnicity.
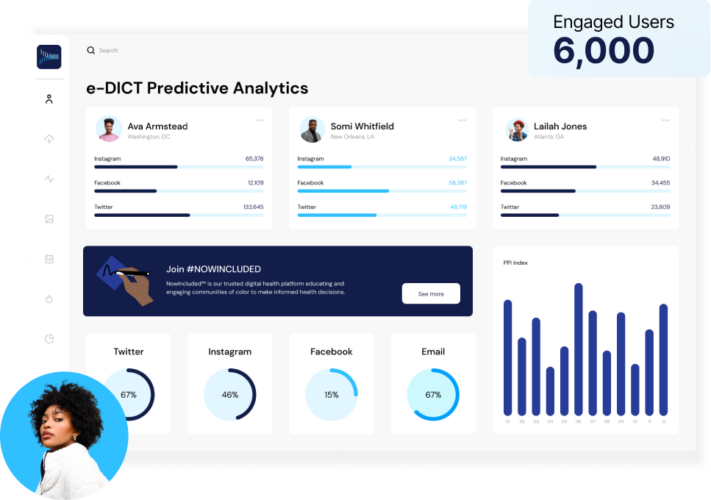
Awareness of this discrepancy is increasing and is being actively addressed by research companies such as Acclinate, which has locations in Birmingham, the HudsonAlpha campus in Huntsville, and Washington, D.C. Co-founded by Del Smith, PhD and Tiffany Whitlow in 2019 after realizing the need to increase diversity in medical trials, Acclinate’s e-DICT platform uses predictive analytics and machine learning to analyze where to find clinical participant leads, accelerating the process of meeting recruitment goals. It partners with pharmaceutical companies, healthcare organizations, and government organizations to ensure they have diverse representation in their clinical studies while minimizing cost and time.
According to Tiffany, they advocate or even enforce that these organizations spend their money differently and invest in early community engagement, locating areas where researchers are likely to find qualified diverse participants for clinical trials and studies.
Acclinate is also working to achieve greater diversity in clinical research trials through its #NOWINCLUDED campaign, which accesses and engages communities of color in conversations with healthcare organizations to modernize clinical trials and boost patient outcomes, as well as to help them make informed healthcare decisions. The campaign features a wealth of resources and allows people to share their stories, including cancer journeys and birth stories.
“For a long time, people felt silenced, and they get so excited when we go into a community and we’re like, ‘we just want to tell your story.’” She also noted that it’s cool to see how it affects people generationally, uncovering previously unknown stories within families and helping open minds based on others’ experiences.
Looking Ahead
Over the next three installments, we’ll cover a variety of issues related to taking control of your health (and your healthcare). Next week, we’ll jump into a few key topics including genetics testing (with a look into some of HudsonAlpha’s latest developments!) and maternal health. We’re all in this journey together – women’s health is essential and there’s no time like now to take action.