Flourish Founder Megan Nivens-Tannett had her first brush with mortality at a very young age when she learned that her grandmother was dying of breast cancer at 54. It was devastating to watch, but she was so young and never really understood the reason for her early death until later in life. Growing up, the word ‘cancer’ seemed to pepper conversations focused on her family’s health and never seemed to escape the family dialogue. Fueled by her mother’s sage advice on proactive healthcare, Megan committed to preventative measures. At 35, she breathed a sigh of relief when genetic tests revealed she was BRCA-negative, dodging what many consider the “ticking time bomb” in women’s health.

4 Generations of Megan’s family.
Flash forward to 2023: While Megan was waiting to be seen for her annual OBGYN appointment, a never-seen-before Nurse treated her and expressed a heightened interest when it came time to review her family history. The Nurse was intrigued, raised her eyebrows, and asked many questions, which took Megan by surprise. She saw her doctor yearly – and there’s never been such a heightened interest in her family history – until now. The Nurse eventually suggested that she take another genetic test, as advancements had come a long way since 2015. The results returned with unwanted information: Megan tested positive for a newly discovered breast cancer marker, the BARD1 mutation. Associated with the BRCA1 gene, the BARD1 gene typically helps prevent cancers, but the mutation increases the lifetime risk of breast cancer by as much as 40 percent. It’s a sobering turn of events, but Megan knows her story isn’t written yet. She has the information, and now she has the power to make informed choices for her future. And in doing so, she aims to rewrite her family’s troubled history with cancer once and for all.
Cars and other vehicles are finely tuned machines with a lot of working parts, and if one of those parts goes bad it can cascade into various and often very expensive and dangerous problems. It’s important to schedule regular maintenance before the dreaded Check Engine light comes on – when problems pop up, ignoring a weird noise or vibration isn’t going to make it go away, and it’s going to cost a lot more to fix it than it would have to prevent it.
Like a car, the human body is also a finely tuned machine requiring regular maintenance and attention to detail. Minor issues might be easy to overlook in the short term, but ignoring changes in your body in the hopes that they’ll go away on their own can lead to major issues down the road. This is particularly important when taking into consideration family history.
According to the National Cancer Institute, there’s good news and bad news about cancer in the U.S: while death rates from cancer have been declining in recent years, the number of new cases have been gradually increasing, especially breast cancer at 0.5% each year.
Breastcancer.org notes that about 13%, or about 1 in 8, women in the U.S. will develop invasive breast cancer in the course of their life. While it’s seen as a women’s disease, men aren’t immune: a man’s lifetime risk of breast cancer is about 1 in 833. The National Breast Cancer Coalition (NBCC) estimates that in 2023, 43,170 women and 530 men will die of breast cancer in the U.S.
The news is worse for women of color: the breast cancer death rate for Black women is 40% higher than it is for White women. In addition, rates of new cases of uterine cancer increased by over 2% a year for every racial and ethnic group except White women, whose rate stabilized from 2014-2018. The National Institute of Health (NIH) attributes this discrepancy in part to socioeconomic status, unequal access to healthcare and housing, and higher rates of aggressive breast cancer subtypes for Black women.
Because cancer has nearly touched everyone in some way, our goal for Breast Cancer and Women’s Health Month is to encourage a proactive approach to self care so that you won’t become another statistic.
Review your family history: There are a number of risk factors that can impact your chances of getting cancer, including age, a lack of physical activity, and alcohol consumption. While some of these are controllable, there’s another one that isn’t: inherited genetic mutations such as BRCA1 and BRCA2. According to the CDC, about 5% to 10% of breast and 10% to 15% of ovarian cancers are hereditary, either inherited from one’s mother or father (or both). For this reason, it’s very helpful to look at the family tree – if multiple people on one or both sides of the family were diagnosed with or died from similar diseases, there’s a much greater chance that you will experience it in your lifetime.
While it may be a difficult topic to bring up, it’s important to have open conversations with your family members to fill in the blanks with medical histories that you may not have been aware of. Here’s a tool to help you start the dialogue.
“It sounds silly, but the women in my family are so in tune with their health that it’s become a regular thing to question what’s on your body. I can remember being at a family get-together and noticing a spot on my Aunt’s shoulder; after discussing it she saw her doctor shortly after, and it turned out to be melanoma. Had she not caught it in time, who knows what would’ve happened.”
— Megan Nivens-Tannett
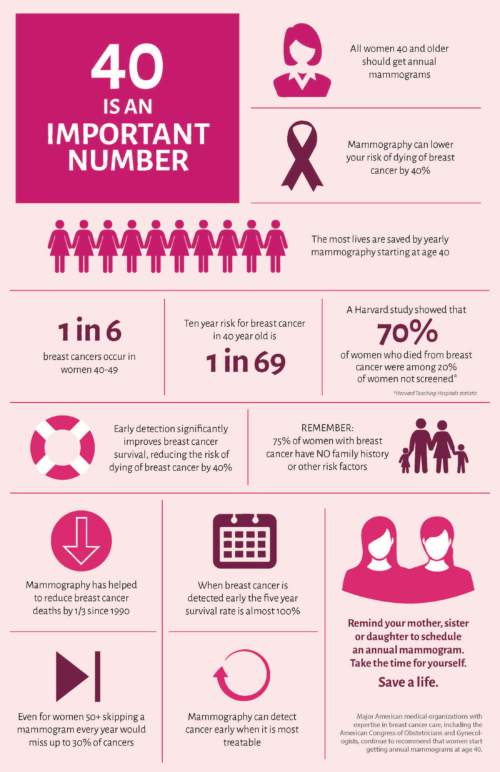
Get screened: The National Cancer Institute notes that by age 30, women have an average of 0.49% chance of breast cancer diagnosis, or 1 in 204. This number increases to 1.55% (1 in 65) by age 40, 2.40% (1 in 42) by age 50, 3.54% (1 in 28) by age 60, and 4.09%, or 1 in 24, by age 70.
In May 2023, the United States Preventive Services Task Force (USPSF) issued a new recommendation lowering the age at which people assigned female at birth should start screening for breast cancer from 50 to 40 years old. The task force recommends that women with average risk factors get screening mammograms every other year from ages 40 to 74.
While younger women can and do get breast cancer, younger women’s breast tissue tends to be denser, resulting in more false positives with mammograms that could result in unnecessary biopsies or surgeries. Instead, regular self exams are recommended for all women aged 20 and older, as well as all men who are at high risk for breast cancer, to monitor for changes. Image Source: Check4cancer.com
Pammie’s Story:
Pammie Jimmar, President of the Greater Limestone Chamber of Commerce, is a testament to the importance of regular screening for the early detection of cancer: in 2018, she went in for a routine mammogram, and after learning that her insurance covered 3D ultrasound imaging, opted for the advanced version. It found a small, suspicious spot, resulting in her doctor ordering a biopsy. It tested positive for cancer. She found an oncologist at Clearview Cancer Institute and together they came up with an initial treatment plan involving sixteen rounds of chemo. Because it was detected early, the cancer hadn’t yet metastasized. Pammie noted that although she had no known family history of breast cancer, she recalled that at the age of 94, her great grandmother had a sore on her breast that refused to heal but never saw a doctor for treatment or diagnosis.
Following the initial diagnosis, Pammie’s tumor started changing in size. Her oncologist presented her with new options: either chemo, radiation, and surgical removal of the spot (lumpectomy), or a mastectomy. She opted for a bilateral mastectomy of the right breast and reconstructive surgery. Looking back following what she described as a fairly smooth recovery process, she has no regrets about her life-saving decision.
When asked what advice she would give to other women, Pammie stated that early detection is key: “It’s your body and God gave us these bodies and He also gave us the wisdom and all of the knowledge and resources out there to use. As a woman, you should be going every year. You should never let anything get in the way of your mammogram schedule – when it’s offered and insurance covers it, definitely do the 3D mammogram because mine was very small, I think 2 cm, but it was cancerous. The 3D mammogram can pick up on even the smallest cancer and that’s when we talk about early detection because if you catch it early enough, it will save your life and you can continue to live a normal, healthy life.”
Pammie also stressed the need for regular self examination, noting that this can help with the discovery of lumps or other irregularities that can then be addressed with a doctor early on.
“It is a very dark time when you’ve been told you have breast cancer. No matter what, when you get the call to say ‘hey, you’ve got breast cancer,’ it’s very daunting. But also, you need to always say ‘get up, dust your knees off, and put on your battle gear’ because then it’s time to fight the battle.”
Pammie has shared her story with many, sharing her experiences and wisdom so that others will be empowered to take control of their own health. She also happened to be featured on our SheBoss series; you can check out the full interview here.
Consider genetic testing: Because not everyone has access to information about their family histories, and even those who do often lack specific details, it can be helpful to tap into recent scientific developments. Ongoing breakthroughs in genetic testing have unlocked a wealth of information on risk factors contributing to higher chances of diagnoses. Genetic testing for BRCA1/2 mutations has been around since 1996, but additional genetic mutations have been uncovered in recent years.
Fortunately, North Alabama has access to a unique resource: Located in Cummings Research Park, HudsonAlpha Institute for Biotechnology is actively working toward pinpointing cancer markers to catch many kinds of cancers before they happen.
Designed to address the need for widespread testing for breast cancer and other cancer markers, HudsonAlpha’s Information is Power Initiative seeks to empower Alabama residents to take control of important health decisions for themselves and their families through noninvasive genetic testing for cancer risk. The screening test is a simple cheek swab, and while it doesn’t replace other types of screening such as mammograms, it does identify changes present in genes that increase the risk for certain types of cancer so that people who test positive can take proactive measures to protect their health.
The Information is Power initiative offers free genetic testing for cancer risk to people ages 28-30 in North Alabama. The initiative is open to all other community members for $129. The test looks for DNA changes in 32 genes that can change your risk for cancer. Participants get their results along with information about what to do next. Genetic counselors help participants and their physicians navigate the question of “What do I do now?” The leaders of Information is Power, Faculty Investigator Dr. Sara Cooper (pictured at right) and Power Project Coordinator Ms. Kristy Bell (pictured at left), are working hard to put this information to work to save lives in North Alabama.
I tested positive! Now what?
First, take a deep breath: a positive result for a cancer marker isn’t a cancer diagnosis or even a guarantee that you’ll get cancer. However, it indicates a significantly greater likelihood that you may be diagnosed with specific types of cancers. . The good news is that if those mutations are found early, action can be taken to decrease or even eliminate the chances of a future diagnosis.
Megan’s story: Aware of her family’s cancer-riddled history, Megan proactively underwent genetic testing at 35 (in addition to performing self-breast exams and never missing an annual appointment!). Despite initial relief from negative results, advancements in genetic testing led her to retest in 2023, unveiling a positive marker for BARD1.
Although not as commonly known as BRCA, a 2019 study of a group of 4469 women found that the BARD1 gene mutation correlates with early onset of breast cancer, faster progression, and a worse prognosis than other forms of breast cancer. Her strong family history of cancers on both sides was a major cause of concern, especially since the BARD1 mutation raises the chance of diagnosis by as much as 40%.
After the initial shock wore off, Megan decided it was time to consider her options so she could make an informed decision. Knowing that her risk was elevated was a good start, increasing her and her doctor’s attention to detail so that minor changes would not be overlooked. A more drastic option was on the table, though: a bilateral risk-reducing mastectomy (BRRM), or the surgical removal of both breasts as a pre-emptive strike to stop cancer before it starts.
The second option comes with its own set of risks – after all, it’s a major surgery that brings major physical changes and a lengthy healing process, especially when paired with breast reconstruction. For some women, such as Angelina Jolie, who lost her mother, grandmother, and aunt to cancer, it was a no-brainer. In her New York Times op-ed, Jolie describes the factors that led to her decision and the process she went through. Most importantly, Jolie notes that thanks to the surgery, her chances of developing breast cancer dropped from 87% to under 5%. “I can tell my children that they don’t need to fear they will lose me to breast cancer.”